Kevorkian faces murder and other charges
In the waning months of 1998, Michigan has finally dealt an emboldened Jack Kevorkian some significant legal blows.
First jury conviction
For the first time in the eight years since he started making headlines by ending lives, a jury has found Kevorkian guilty of a crime. On 11/4/98, the day after Michigan voters rejected a measure to legalize assisted suicide, the state’s foremost death advocate was found guilty of misdemeanor assault and resisting arrest. The charges stemmed from a scuffle with police outside a Royal Oak hospital on 5/7/98 when Kevorkian and his sidekick, psychiatrist Dr. Georges Reding, dropped off the body of 26-year-old Matt Johnson, a quadriplegic from California. (See Update, 7-10/98:8.) Prior to this guilty verdict, Kevorkian had been acquitted by three juries in other cases, while a fourth jury trial in 1997 ended in a mistrial.
But in this case, jurors held Kevorkian accountable. “Kevorkian was out of control,” explained jury foreman Gerald Arbenowski. “He should have just called his lawyer.” Reding, according to the jury, was not guilty of the charges.
True to form, Kevorkian verbally attacked the jury, calling the four women and two men pawns in a conspiracy against him, comprised of government forces, police, and media. “The jury was intimidated by those crooks,” Kevorkian declared. When told of Kevorkian‘s claim, juror Dawn Mullen replied, “No, we’re not. We have our own opinions.” [Detroit News, 11/5/98; Detroit Free Press, 11/5/98; AP, 11/4/98]
Royal Oak District Judge Daniel Sawicki ordered Kevorkian to immediately pay $700 in fines and $200 in court costs or spend 60 days in prison. Despite his empty demands to be sent to prison for the “maximum penalty,” Kevorkian decided to have his friend, Neal Nicol, pay the fines and costs because, he said, “I have things I have to do.” [Detroit News, 11/5/98]
The judge also sentenced Kevorkian to two years probation, during which time he is not allowed to violate any law or ordinance. Later, Kevorkian asked reporters, “You think I’m going to obey the law?” “You’re crazy,” he boasted. [AP, 11/5/98; Reuters, 11/4/98] At that moment, though, Kevorkian knew something that the reporters and the rest of the world did not. He had already committed the ultimate crime, and had videotaped it for recorded history.
Packaging murder
Now the biggest question facing the publicity-seeking death doctor was how to get the most attention and media coverage for his latest bombshell: the 9/17/98 killing of 52-year-old Thomas Youk, a Waterford Township resident with Lou Gehrig’s disease (ALS). It was on 11/4/98 — the very day he was convicted of assault and resisting arrest, the very day he decided to pay the fines instead of going to jail because he had “things… to do” — that Kevorkian contacted Mike Wallace of CBS’ 60 Minutes.
Kevorkian offered Wallace, a known assisted-suicide supporter, an exclusive, complete with two videotapes, one of Youk’s actual death, the second of an earlier interview with the soon-to-be-dead “subject” (Kevorkian’s own term). Wallace and executive producer Don Hewitt decided to air segments of the tapes and give Kevorkian the platform he wanted. They scheduled the broadcast for 11/22/98 — the last Sunday of the November “sweeps,” the highly competitive network ratings race upon which advertising rates are based. The Kevorkian segment garnered for 60 Minutes the season’s best rating (more than 15.3 million households watched Youk die) and was responsible for putting CBS ahead of NBC for overall supremacy. [AP, 11/27/98]
Those who viewed the 60 Minutes broadcast saw Youk sitting in a wheelchair, depressed, hopeless and, as Kevorkian described him, “He was terrified of choking — terrified.” Later Kevorkian explained to Wallace, “He just was terrified of—he was very afraid of choking to death, and he must have felt that he was on the verge of it. And I couldn’t have him suffer in that kind of frame of mind because if the man is terrified, it’s up to me to dispel that terror.” [Transcript, “Death by Doctor,” 60 Minutes, 11/22/98]
Instead of pressing Kevorkian about available ways to help Youk rather than kill him, Wallace, usually a tough interviewer, simply murmured, “Mm-hmm,” in assent. There was no mention of the fact that, with proper treatment and care, ALS patients do not choke or suffocate. Nor did Wallace pick up on Kevorkian’s revealing statement that, in his incredibly self-absorbed view, it was up to him alone “to dispel [Youk’s] terror.” Wallace simply accepted Kevorkian’s false premise that Youk had only two options: choke or let Kevorkian kill him.
According to IAETF lawyer and hospice volunteer Wesley J. Smith, “It was unconscionably cruel of Wallace to allow Kevorkian’s propaganda to go unchallenged.” In a recent article for The Weekly Standard, Smith wrote, “One expert Wallace could have interviewed is Dr. Walter R. Hunter, a medical director of Hospice of Michigan…. Hunter was appalled at the depiction of Lou Gehrig’s disease presented on 60 Minutes. ‘No one with ALS should be allowed to choke,’ Hunter told me.” There are medications to control secretions, simple suction devices similar to those used in dentist offices, oxygen machines, and low doses of morphine — all very effective in keeping ALS patients comfortable. [Wesley J. Smith, “Lying about Dying,” The Weekly Standard, 12/14/98:14]
It was evident throughout the videotaped excerpts aired by CBS that Kevorkian was clearly in charge of the Youk situation. He decided that Youk would die from lethal injections he administered, rather than Youk ending his own life by triggering Kevorkian’s infamous “suicide machine.” Wallace told viewers, “Kevorkian suggested that instead he give Tom a lethal injection. He says that’s more reliable and more humane, and he wants to push the public debate from doctor-assisted suicide to euthanasia.” Turning to Kevorkian, Wallace asked, “Did Tom know that you were making, in effect, an example [of him]?” “Yes,” Kevorkian replied. “And I sensed some reluctance in him. I—I did.” When Wallace asked, “How do you know he agreed?” Kevorkian recalled, “I had him sign, saying that he chose direct injection.” [Transcript, 60 Minutes]
The tapes also revealed Kevorkian’s cold, unfeeling, and businesslike manner. Just like in the case of his first victim, Janet Adkins in 1990, and others, the unemployed pathologist had difficulty finding a vein. After a number of unsuccessful attempts, he eventually decided to inject Youk in the tender area between the fingers of his right hand. Talking directly to Youk, Kevorkian matter-of-factly announced, “And we’re ready to inject! We’re going to inject in your right arm. OK? Okey-doke.” After showing the tape of Kevorkian giving Youk a lethal series of three injections, Wallace told viewers, “He’s dead,” to which Kevorkian added, “Yep. The heart has stopped.” [Transcript, 60 Minutes]
During an interview with Kevorkian sympathizer and freelance reporter Jack Lessenberry—to whom Kevorkian showed his tapes prior to giving them to Wallace—Kevorkian explained that Youk’s death had not gone all that smoothly. In addition to being nervous and unable to find a vein, Kevorkian told Lessenberry, “See, I used an EKG on this one also, but I put the paper in backward and had to pull it through by hand.” According to the reporter, Kevorkian then exhibited “a slightly bloodstained scroll of paper whose squiggles seem to show a heart beating and then flat-lining.” When Kevorkian was asked if Youk had anything to say at the end, Kevorkian laughed and said, “I don’t know. I never understood a thing he said.” [Jack Lessenberry, “I want a showdown,” Oakland Press, 11/20/98:A1]
Kevorkian charged with murder
Based on the Youk videotapes, a Michigan judge has ordered Kevorkian to stand trial for first-degree murder, assisted suicide, and delivery of a controlled substance. Referring to the fact that Kevorkian acted with premeditation, Judge Phyllis McMillan said, “It was clear that Dr. Kevorkian planned to help Mr. Youk end his life over the course of a few days.” “This was not the result of a sudden impulse or anything of that nature…,” she added. [Court TV, 12/9/98; Reuters, 12/9/98]
The mandatory sentence for first-degree murder is life in prison. The assisted-suicide charge—under Michigan’s newly enacted law banning the practice—carries a sentence up to five years and a $10,000 fine. The penalty for the third charge, delivering a controlled substance, is up to seven years. Kevorkian has pleaded not guilty. [AP, 12/9/98, 12/17/98]
The trial date has been set for 3/1/98. The judge will be Jessica Cooper, who presided over a previous Kevorkian trial in 1996 that ended in acquittal. The prosecutor will also be the same one from the 1996 trial, John Skrzynski. But, according to reports so far, longtime Kevorkian attorney Geoffrey Fieger will not be at the defense table. Fieger gave up his infamous client to run for governor. While he was defeated by a vote of 38% to 62%, Fieger now has a new radio show and is considering running for mayor of Detroit. He has, however, offered to rescue Kevorkian if need be. [Detroit News, 12/10/98; Detroit Free Press, 12/3/98]
State to charge Kevorkian, too
State officials have indicated that they are reviewing the Youk tapes in preparation for charging Kevorkian with contempt and practicing medicine without a license. Last year, the state issued a cease-and-desist order to stop the unlicensed Kevorkian from practicing as a physician, an order which Kevorkian publicly set on fire. “We plan to go forward in January to enforce the cease-and-desist order,” said Kathy Wilbur, Consumer and Industry Services director. “It’s very clear he violated the law by practicing medicine,” she added. [Detroit News, 12/23/98]
Michigan voters overwhelmingly reject assisted suicide measure
On November 3, 1998, in what can only be described as a trouncing, voters in Michigan overwhelmingly defeated Proposal B, the ballot measure which would have made it legal for doctors to intentionally prescribe lethal drugs to kill certain patients. If passed, Proposal B would have overturned Michigan’s newly enacted assisted-suicide law banning the practice. Instead, voters soundly rejected Proposal B by a vote of 71% to 29%.
“We’re grateful that Michigan voters realized [Proposal B] would have created a lot of problems and voted ‘no,’” by more than a 2 to 1 margin, said Michigan Medical Society President Dr. Cathy Blight. Blight was co-chair of Citizens for Compassionate Care (CCC), a broad coalition of individuals and organizations opposed to the measure which raised over $5.5 million for the “B is Bad” campaign.
By contrast, Merian’s Friends, Proposal B’s sponsoring group, was able to raise only $75,000 for television ads. “We started out the race being well ahead, and what happened was we went broke,” said Dr. Ed Pierce, Merian’s Friends’ chairman and former state senator. “If we could have defended ourselves through 30-second spots on TV, we would have won,” Pierce speculated. [Michigan Daily, 11/4/98]
But Dr. Blight would disagree that money alone was the determining factor in the campaign. “The real story behind this victory is the grassroots nature of this campaign,” she explained.
“When thousands of doctors began saying, ‘B is Bad,’ it affected their families, staffs, and patients…. The hospice movement’s unequivocal message against B moved thousands of votes. The disability rights community denounced Proposal B, and their circle of influence pushed thousands more NO votes. When Jewish, Muslim, Protestant and Catholic leaders spoke out for true compassion, hundreds of thousands took it to heart. You cannot drive anywhere in the state without seeing a flood of ‘NO on B‘ yard signs. That‘s a telling expression of citizen democracy. This was a campaign by the people, for the people.” [CCC, Press Release, 11/3/98]
Noted University of Michigan law professor Yale Kamisar discussed another perspective on the landslide defeat of Proposal B in a recent New York Times op-ed piece. According to Kamisar, “The Michigan experience shows that it is much easier to sell the basic notion of assisted suicide than to sell a complex statute making the idea law.” “When pollsters ask about the issue, most people, I suspect, focus on the poignant case,” he wrote. “But when people are asked to approve a complex, 12,000-word initiative, as in Michigan, the focus shifts. Now people start worrying about whether the measure provides too few procedural safeguards, or too many. They worry about whether it would impose too many burdensome requirements on dying patients and their loved ones.” Quoting ethicist Sissela Bok, Kamisar added, “’No society has yet worked out the hardest questions of how to help those patients who desire to die, without endangering others who do not.’” [Kamisar, “Details Doom Assisted-Suicide Measures,” New York Times, 11/4/98]
Among those most endangered by the legalization of assisted suicide and euthanasia are individuals with disabilities. Members of the disability rights group Not Dead Yet have often advocated for a legal prohibition to Jack Kevorkian’s induced-death “practice” and actively opposed Proposal B as “inherently discriminatory, singling out the older, ill or disabled as less valuable.” “Unlike referenda in other states which ended in very close votes, Michigan voters have already seen the future when the door to so-called assisted suicide is opened,” observed Bob Liston, coordinator for Not Dead Yet’s Michigan branch. “We believe that the parade of deaths orchestrated by Jack Kevorkian had a definite impact on Michigan voters — and they answered with a resounding ‘no’ to legalization,” he said. [Not Dead Yet, Press Release, 11/4/98]
While Michigan voters do not want “death bureaucracies or manipulations of vulnerable patients,” Dr. Blight explained, they do want “compassion and comfort for those facing their final days.” “We must set our sights on a new campaign,” she said, “that will ensure that the citizens of Michigan have access to all appropriate care at the end of life.” [CCC, Press Release, 11/3/98]
With that goal in mind, the CCC coalition spent an additional $200,000 after the election for TV airtime to run ads informing the public about alternatives to assisted suicide. Kevin Kelly, managing director of the Michigan State Medical Society, called the new campaign theme “physician-assisted living.” The coalition, he said, is convinced that, if people had more help dealing with terminal illness, they would not give assisted suicide a thought. [The Oakland Press (MI), 11/14/98:A6] As Dr. Walter Hunter of Hospice of Michigan succinctly put it, “I don’t want to ever see this on the ballot again.” [Detroit Free Press, 11/4/98]
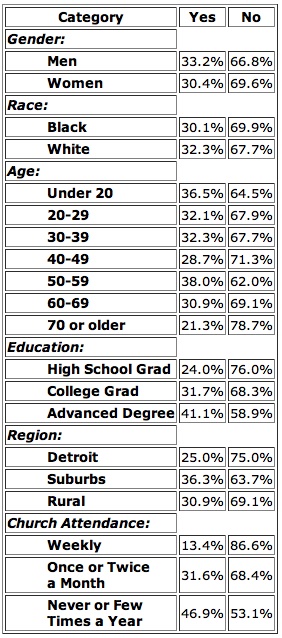
Proposal B Vote Demographics
Source: Detroit News exit poll of 2,235 voters on 11/3/98. Margin of error: ± 3 percentage points. Detroit News, 11/4/98.
Oregon adopts official policy to cover assisted-suicide costs
One year after the nation’s only law permitting assisted suicide took effect, state officials in Oregon have adopted a policy to cover the costs of legally ending the lives of low-income Oregonians. Last February, the Oregon Health Services Commission voted to include assisted suicide as a covered “medical service” for 270,000 low-income residents under the state’s unique Medicaid health care rationing program. It added assisted suicide to the “comfort care” treatment category for any “terminal illness, regardless of diagnosis.” (See Update, 1-3/98)
On 11/30/98, state Health Plan officials upheld that policy, reaffirming the position, according to Associated Press, that Oregon’s poor “should be able to choose death at taxpayer expense.” [AP, 12/2/98] Officials estimated that the state would pay less than $45 for the lethal drug prescription, between $9 to $81 for each doctor’s office visit, and between $30 to $118 for each counseling session, if necessary. “In the grand scheme of things,” said Lynn Read of Medical Assistance Programs, “this doesn’t compare to some of the surgical procedures and other things that we pay for.”
“The fact that the state of Oregon will not properly fund our personal attendant services, yet will pay for us to die, amounts to nothing less than cultural genocide,” said Ric Burger, a diabetic, wheelchair user, and president of the Oregon chapter of the American Disabled for Attendant Programs Today (ADAPT). [Oregonian, 11/24/98]
Futile Care: Who Decides?
by Wesley J. Smith
Imagine your husband is in a hospital, struggling against a debilitating or life-threatening disease. If something goes wrong, you tell the doctor to do what he can because your husband wants to live. But the doctor says no, he does not believe that the quality of your husband’s life is worth doing as you ask. Indeed, he is so adamant, he puts a Do Not Resuscitate (DNR) order on your husband’s medical chart over your objections, meaning that if he suffers a cardiac arrest or some other life-threatening event, he plans to stand by idly and watch your husband die.
Frightening stuff. Unfortunately, it is also true. This is close to what befell Andrew Sawatzky, 79, of Winnipeg, a resident at the Riverview Health Centre since May. Sawatzky has had strokes and has advanced Parkinson’s disease. Helene, his wife, says her husband can communicate (this is disputed by doctors) and wants to live as long as he can. Moreover, their religious faith requires continued care.
If Sawatzky has a heart attack, Helene wants him to have CPR. But she was told by Riverview that they won’t do it, that CPR would be “futile.” Over Helene’s objections, a DNR order was entered upon his medical chart. She sued to require his own doctors to treat him in a medical emergency. On November 11, she won a victory. But it is only temporary, pending court proceedings.
In a similar case, a Quebec man didn’t survive long enough to take his doctors to court. Earlier this year, Herman Krausz, 76, was admitted to Montreal Jewish General Hospital, in respiratory distress from a lung infection. At first, he improved; then he developed pneumonia and had to be put on a respirator.
According to his family, Krausz, who was not unconscious or incompetent, knew he would probably last only a few weeks. Still, he wanted to continue to receive respiratory support so he could spend his remaining time with his family. According to Krausz’ family, that did not sit well with the intensive care medical director who ordered the respirator turned off against his patient’s and the family’s wishes. Krausz died 15 hours after he was taken off the respirator. The matter is now set for a coroner’s inquest.
Ironically, most people are more worried about being “hooked up to machines” against their will than of being denied wanted medical care. That is because in too many cases, doctors used to keep people alive regardless of their desires. But that danger faded substantially after medical ethicists successfully argued that patients should be allowed to re-fuse unwanted medical treatment even if ceasing care would lead to death. As a result, patient autonomy became a mainstay ethic of medicine.
Under the principle of patient autonomy, if Sawatzky wanted a DNR order placed on his chart, that was his right. Similarly, if Krausz had wanted his respirator turned off, that would have been done. So, one would suppose that these men had a similar right to receive treatment. Autonomy is autonomy, right?
Not necessarily. Increasingly, when it comes to end of life care, patient autonomy is a one-way street toward death. If a patient refuses care, the decision is sacrosanct. But if the patient’s “choice” is for treatment such as CPR, antibiotics, ventilator, feeding tube, or blood transfusion in order to stay alive, we are told by some doctors, medical ethicists, and health care cost utilitarians that autonomy has its limits. Treatment requests they view as “inappropriate” will be refused.
This heads-I-win, tails-you-lose philosophy is known generically as Futile Care Theory. To fully comprehend the wickedness at work here, it is important to understand how medical ethicists have turned the traditional concept of medical futility on its head. A futile intervention used to be defined as one that had no possible physiological benefit. To use an extreme example to illustrate the point, if you asked your doctor to remove your appendix to cure an ear infection, the doctor should refuse because the surgery could not benefit you medically and would harm you.
In contrast, futile care (also called “inappropriate care”) is about subjective value judgments by medical professionals rather than physiological outcomes. Sawatzky’s involuntary DNR order was imposed not because CPR would have no physical benefit, but because it might. Similarly, Krausz’s respirator was turned off against his will not because it wasn’t benefiting him—but because it was. Thus, it isn’t the proposed treatments that were deemed futile in these cases, but the patients. Bluntly stated, Sawatzky and Krausz were seen as people who should die.
Throughout Canada and the U.S., hospitals and medical associations are quietly adopting formal futile care policies with which to browbeat families and patients who want “inappropriate” care and to convince courts to permit doctors’ and medical ethicists’ values to prevail over patient and family decision making. This is nothing less than the modern equivalent of exposing unwanted infants on hills and abandoning the infirm and elderly by the side of the trail.
A case in Spokane, Washington, demonstrates just how dangerous all of this really is. On October 27, 1994, Baby Ryan was born prematurely at 23 weeks gestation. He was put on dialysis, but the doctors determined that continuing treatment was “futile” and they halted it over his parents objections. Ryan would have died, but his parents obtained a court order to continue his treatment.
Administrators and doctors fought the parents in court swearing under oath that “Ryan’s condition is universally fatal” and that the infant had “no chance” for survival, contending that Ryan’s continued treatment was a violation of their integrity, values and ethics. The court never decided who had ultimate say over Ryan’s care — his parents or the hospital — because he was transferred to Emanuel Children’s Hospital in Portland, Oregon, where he was soon weaned off dialysis and survived.
Had his original doctors successfully imposed their values on their patient, Ryan would be dead today. Instead, he is a living four-year old child. If patient autonomy is to have any meaning other than providing a veneer of respectability for a “duty to die,” the futile care movement must be stopped. Our lives and dignity— and that of those we love— depends on it.
Wesley J. Smith is an attorney for the IAETF and the author of Forced Exit: The Slippery Slope from Assisted Suicide to Legalized Murder, published in 1997 by Times Books/Random House. His article originally appeared in Canada’s National Post (11/23/98:A14), and is reprinted here with the author’s permission.
Productive in His Own Way
by George T. Crane
Productive members of society.
This is what most education, training and employment programs for disabled people are intended to create. It is a good and noble purpose that has, quite literally, opened doors for many. Whatever good it may bring, however, this utilitarian approach could be fatally flawed if crudely applied to the medical care of all disabled people. It would tolerate, perhaps even condone, the death of my son.
Aidan is severely disabled, the result of a rare combination of brain abnormalities. Now 6 years old, he is more like an infant: he cannot hold his head upright; he cannot crawl, walk or talk. The seizures that fire through his brain have proved incurable after a dozen or more medications. He is profoundly mentally retarded. We feed him through a tube that runs directly into his small intestine, to avoid aspiration pneumonia. The visual world is, for him, a dim play of shadows.
It would seem, then, that Aidan is not and will never be a “productive member of society.” Insurance companies are especially frustrated by Aidan’s lack of productivity. His care is expensive, with many hospital stays, regular visits to various doctors and more than $1,000 in food bills a month. Once, when a nurse friend of ours was arguing to an agent of a health maintenance organization that she should continue her visits to Aidan, the agent complained that it was the parents’ fault, all of this expense, for “keeping these kids alive.” Care for Aidan, the agent implied, was socially irresponsible because it took resources away from other, more promising and profitable uses.
These agents press at us constantly, saying that the formula specially made to suit his tube-feeding is not ‘medically necessary,” and therefore not covered. Or they balk at authorizing a referral to yet another specialist. They think that Aidan’s limited prospects are just not worth the work and anguish.
But Aidan is worth it. His value comes precisely from the challenge he poses to the usual definitions of “value.” He is a living reminder that the range of human experience is broader than the narrow confines of balance sheets and business plans. While he will never pay back society in financial terms, he certainly gives to those around him.
To my wife and me he has given the gift of perspective. A good day now is not a matter of more income or greater social status or new things from the mall, but a time of fewer seizures or his comfortable sleep in his own bed. He has expanded the world of his little sister, Margaret. Though only 4, she is not afraid of wheelchairs or white canes; she knows that not everyone walks or talks or sees.
He has a similar impact on his friends at school—yes, he is entitled by law to be included in the local public school. His classmates were put off at first by the wheelchair, the seizures, the strangeness. But after a simple explanation—”he was just born that way”—they come to accept him, even compete to push his chair or hold his hand. Some have forged real friendships with him, asking to trick-or-treat with him at Halloween or inviting him to a birthday party.
His most profound effect, however, is the reflection he inspires in many who meet him. Without a word, he poses the deepest questions. What is a life? What makes any life, even one so limited, worth it? Strangers have come up on crowded streets, touching his shoulder or tousling his hair, giving us their abbreviated answers. Usually they say something about love or grace, something well beyond the material concerns of everyday life. With Aidan, it’s never about productivity, it is about humanity.
George T. Crane teaches political science at Williams College in Williamstown, Massachusetts. His article originally appeared in the New York Times, November 30, 1998. It is reprinted here with permission. Copyright © 1998, by the New York Times.
World Focus
AUSTRALIA
Australian doctor claims 15 euthanasia deaths
Borrowing from the publicity tactics of America’s Jack Kevorkian, Dr. Philip Nitschke, often referred to as Australia’s Dr. Death, has announced that he has a library of at least 15 videotapes showing people whose lives he has claimed. His announcement came within the week following 60 Minutes’ broadcast in the U.S. of Kevorkian’s videotape of Thomas Youk’s death. “What Kevorkian has done is incredibly brave,” Nitschke told reporters, “but I don’t have that sort of courage.”
Nitschke indicated that he hoped his tapes, unlike Kevorkian’s, would protect him from prosecution, not provoke it. But Australian Medical Association spokesman Gerald Segal said Nitschke should be charged. “If he’s got videos, I would be strongly suggesting that he was committing illegal acts,” Segal explained.
The tapes, according to Nitschke, are testimonials in which the patients say that they want to die and want Nitschke’s help in doing so. He plans to use the tapes to sway juries, if he were ever prosecuted in court. “The only time these videos will see the light of day would be if I was misfortunate enough to find myself in front of a jury,” he told reporters. [AP, 11/28/98]
Nitschke, of course, is not new to the induced death spotlight. He was responsible for the four legal euthanasia deaths under the now overturned Northern Territory euthanasia law. He also developed a computer program, (See Update (4/96) and Update (10-11/96)) available on the Internet, designed to kill patients by delivering lethal drugs through an intravenous line, as well as a “suicide pill” composed of common household ingredients. Earlier this year, Nitschke announced plans to open a euthanasia clinic in Melbourne to put, among other things, despairing patients in touch with black market sources for barbiturates and other drugs. (See Update, 7-10/98)
……..
CANADA
Latimer’s light sentence overturned
The Saskatchewan Court of Appeal has overturned a lower court’s lenient sentence in the Robert Latimer case. Latimer, 45, was convicted twice of second-degree murder in the death of his disabled twelve-year-old daughter, Tracy, whom he placed in the cab of his truck and gassed to death by hooking up tubes and pipes to the truck’s exhaust system.
The first conviction in 1994 was dismissed on a technicality. The second conviction carried a mandatory life sentence with no chance of parole for 10 years. Police records indicated that Latimer had, with premeditation, planned Tracy’s death, and had told police that he decided to gas his daughter to death after rejecting earlier plans of shooting her in the head and setting her body on fire.
He claimed in court that he just wanted to end her suffering. While Tracy had severe cerebral palsy, routine surgery to relieve her pain had been scheduled—but her father killed her before she could benefit from the highly successful treatment.
The second trial judge, Justice Ted Noble was moved by Latimer’s claims and, instead of giving him the mandatory life sentence with no possibility for parole for 10 years, granted Latimer a rare constitutional exemption. Latimer had killed his daughter out of “mercy,” the judge ruled, and the mandatory 10-year sentence would be cruel and unusual punishment. Instead, Judge Noble sentenced Latimer to only two years less one day, the first year to be served in jail, the second at home on his farm. Latimer has remained free pending further appeals. (See Update, 11-12/94:7 and Update 11-12/97)
On 11/23/98 the Saskatchewan Court of Appeal unanimously ruled that Judge Noble went beyond his authority in granting Latimer a constitutional exemption from the mandatory sentence. “The recommendation was not only uninformed, but it also has no legal effect,” Justice Stuart Cameron wrote in the court’s 34-page decision. “Mr. Latimer is answerable for the inexcusable murder of Tracy Latimer, a murder which has been classified by Parliament, for sentencing purposes, as second degree.”
Latimer is currently free on bail pending an appeal to the Canadian Supreme Court. However, since the decision by the Saskatchewan appellate court was unanimous, Canada’s Supreme Court can refuse to hear Latimer’s appeal. [National Post, 11/24/98; Globe and Mail, 11/24/98; New York Times, 11/24/98; Canadian Press, 11/23/98]
……..
Crown drops murder case against Canadian doctor
Government prosecutors have dropped their case against Dr. Nancy Morrison, a Halifax respirologist who had been charged 18 months ago with the 1996 murder of Paul Mills, a terminally-ill patient in her care. Earlier this year, the first-degree murder charge against Morrison had been dismissed by Nova Scotia Provincial Judge Hughes Randall, saying that the prosecution had failed to make its case that Morrison had given Mills a lethal intravenous injection of potassium chloride. Mills allegedly was within hours of dying naturally and was in great pain. “I don’t think that she meant to murder him. I think she meant to alleviate the pain,” said Calixte Mills, the patient‘s brother. “Nobody ever convinced me that Dr. Morrison meant to kill my brother.”
The Crown appealed Judge Randall’s dismissal of the case, but the Nova Scotia Supreme Court concurred with his ruling. [National Post, 11/20/98] “The Crown will discontinue all criminal proceedings against Halifax physician Dr. Nancy Morrison,” Crown attorney Craig Botterill told reporters. “We believe the criminal case has run its full course…. We’ve carefully reviewed the decision of the Supreme Court review and have concluded that there’s no reasonable likelihood that a further appeal would be successful.” But Botterill also warned that the Crown has an obligation to uphold the law prohibiting mercy killing. “I hope the message that comes from this prosecution is loud and clear, and that is: The police and the Crown in this province respect the law as given to it by Parliament and that we have and will continue to prosecute—to the fullest extent of the law—mercy killing,” he explained. [Canadian Press, 12/11/98; AP, 12/12/98]
……..
ENGLAND
British psychiatrists polled on euthanasia
A national survey of 322 psychiatrists in the U.K. revealed that four out of ten think that it should be legal for physicians to help terminally-ill patients commit suicide. Almost one in three thought it was sometimes justified for a physician to actively end a patient’s life. Approximately 86% indicated that for some patients committing suicide was a rational act. But only one-third answered yes when asked if they would be willing to assess patients’ mental states if they wanted to die. According to lead researcher Dr. James Warner, psychiatrists are very cautious about taking an active role in the practice of inducing death. “They are trying to save life and to be involved in a process that is going to end a person’s life could leave an uncomfortable taste in the mouth,” he said. Warner also explained that psychiatrists are often too busy to assess patients who express a death wish. “To assess whether a patient was mentally ill would not be something that could be done in an hour’s consultation,” he said. “It would require a very long assessment process, and psychiatrists do not have the time to do it.” [The Lancet, 10/24/98:1360; BBC News, 10/22/98]
Coma patient’s experience highlights danger of euthanasia
After an accident left Joan Smith (not her real name) in a coma, she was completely paralyzed but could hear all that was going on around her. According to the 42-year-old business woman, “I could hear the doctors discussing me, so I knew how ill I was. I heard them saying that my lungs were full of poison and there wasn’t much hope.” “Twice a priest came into the room and gave me the last rites,” she said.
Her biggest shock, however, came while she was on a respirator and she heard her husband telling the doctors that the respirator should be turned off because his wife would not want to live under these circumstances. “My husband was issuing my death sentence—I wanted to scream,” she recalled, but couldn’t. It was only because of her daughter’s persistence that her treatment continued, allowing her to fully recover. [The Sunday London Times, 12/15/98]
British doctor pleads not guilty in euthanasia case
British physician David Moor, 51, has pleaded not guilty to the murder of one of his cancer patients, 85-year-old George Liddell, who died in July 1997. Liddell’s scheduled cremation was stopped by authorities after Moor told reporters that he had helped as many as 150 patients die over the course of his 30-year medical career. Moor described the most recent patient whose death he induced as having bowel cancer and “slowly dying” for three months. Liddell fit that description. (See Update, 4-6/98) Moor was charged with murder after drug tests were ordered on Liddell’s body. He is scheduled to go on trial next April. [BBC News, 10/18/98]
……..
NETHERLANDS
Dutch physician says euthanasia abuse widespread
Dutch palliative care doctor Dr. Ben Zylicz recently told those gathered at the United Kingdom’s House of Lords that euthanasia practice in his country is detrimental to good medical practice. The instances of involuntary or non-voluntary euthanasia, he reported, are becoming widespread, and in violation of formal Dutch guidelines and safeguards.
According to Zylicz, the reason doctors (and patients) often resort to euthanasia is that adequate palliative care is not easy to obtain, with only 70 specialist palliative care beds in the entire country. Moreover, few Dutch physicians have been trained in pain management and symptom control and, consequently, euthanasia is the only solution they know if the patient’s suffering becomes too great.
“If you accept euthanasia as a solution to difficult and unresolved problems in palliative care,” he explained, “you will never learn anything.” Most disturbing, Zylicz warned, is how often the euthanasia guidelines, established to protect against abuses, are breached by doctors. In 1995, he said, there were 900 cases of non-voluntary euthanasia reported. As many as 25 percent of those patients were killed without requesting death, even though they were fully or partly competent.
Professor Lord McColl, Lords Select Committee on Euthanasia member, added to Zylicz’s testimony by relating his reaction while on an official trip to the Netherlands. “Our visit convinced me that euthanasia is impossible to police and will be abused,” he said. [British Medical Journal, 12/12/98]
……..
NEW ZEALAND
New Zealand sets precedent in “futile care” case
The High Court of Auckland recently granted doctors the authority to remove life support from a severely disabled infant despite the parents’ strong opposition. The infant, referred to as Baby L, was born two months prematurely and, according to the doctors, had cerebral palsy, was blind, deaf, severely brain-damaged, and unable to breathe without a ventilator. The parents lost their fight after the High Court made Baby L a ward of the court. Two of the judges ruled that, while the parents’ wishes should be taken into account, they had no veto authority. The hospital took the case to court after its ethics committee determined that the infant’s situation was “hopeless” and that her treatment was “futile and therefore inhumane.”
The court’s ruling caused the disability rights community and others to condemn the decision as fostering infanticide. Christian Heritage Party head Graham Capill commented, “It is all too easy to look at the quality of life rather than compatibility with life.” [London Telegraph, 9/26/98]
……..
SWITZERLAND
Distress declared justification for assisted suicide and euthanasia
Eighteen medical professionals — attending the 12th International Conference of the World Federation of Right to Die Societies, held in Zurich last October — have signed a document pledging their support for the legalization of assisted suicide and euthanasia, and stipulating that “distress,” not illness, is sufficient justification for ending a person’s life. The document, entitled the “Zurich Declaration on Assisted Dying,” clearly states, “We believe that we have a major responsibility for ensuring that it becomes legally possible for all competent adults, suffering severe and enduring distress, to receive medical help to die….” [Emphasis added.] According to IAETF Executive Director Rita Marker, “One who is experiencing physical, mental, emotional, economic, or familial problems would qualify for a fatal overdose or a lethal injection as long as the distress from such factors is considered ‘severe and enduring.’”
The declaration also supports the inclusion of medically assisted death as a comfort care option, an option which should be available, they say, even if the patient is receiving outstanding pain and symptom control. “Excellent palliative care should not exclude the right to choose assisted dying,” the document states. [“Zurich Declaration on Assisted Dying,” 10/14/98]
News Notes
Dr. Eugene Turner, a popular pediatrician in rural Port Angeles, Washington, has been charged with second-degree murder in the 1/12/98 death of 3-day-old Conor McInnerney. While Turner has admitted that he placed his hand over the baby’s nose and mouth blocking the infant’s airways, he has formally pleaded not guilty to the murder charge.
The newborn had been rushed to Olympic Memorial Hospital after his parents noticed that he had stopped breathing. The emergency room (ER) doctors were able to get the infant’s heart beating again, but the baby remained limp, with his pupils fixed and dilated. The parents agreed to stop life-support, and the baby was pronounced dead. But, about 30 minutes later, a nurse returned to the ER and noticed that the infant was gasping for air and that his skin was turning pink. Turner rushed back to the ER, but instructed the staff not to call the baby’s parents. He reportedly said that he wanted to save the parents from having to watch their son die twice. (See Update, 1-3/98)
Turner and another ER doctor continued to work on the infant for two more hours, after which Turner suddenly declared the child brain dead and suffocated him by obstructing his nose and mouth. According to one of the nurses, “Dr. Turner said, ‘I can’t stand it, I can’t have this go on anymore.” “I saw him plugging off the infant’s nose,” the nurse recalled. “We were shocked, numb.”
Turner claims that he was just stopping the baby’s “reflexive” or “agonal” breathing—after the infant was already dead. But Michelle McInnerney, the infant’s mother, told a TV interviewer, “As far as I’m concerned, Conor was coming back. God was working a miracle for Conor and for us.” She said that “none of this would be going on today” if Turner had not blocked the baby’s airways. “We’d have Conor with us, and he’d be playing right now.” [AP, 8/31/98; AP, 2/23/98]
Earlier this year, the state Medical Quality Assurance Commission charged Turner with unprofessional conduct. He has surrendered his hospital privileges at Olympic Memorial, but continues to see patients in his private practice. His trial on second-degree murder is scheduled for January 25, 1999. [AP, 12/10/98]
……..
Derek Humphry, a founder of the pro-euthanasia Hemlock Society and author of the how-to suicide manual, Final Exit, has a new book out entitled, Freedom to Die. In it, Humphry writes that “in the final analysis economics will drive assisted suicide to the plateau of acceptable practice.” When asked on ABC’s Good Morning America what he meant by that, Humphry stated,
“Some people are intelligent and rational. They are suffering, they are dying, there’s no quality of life left. If they want to kill themselves, why shouldn’t they be allowed to? Why waste valuable health dollars on people who want to go when that money would be better spent on poor children or poor people or medical experimental testing and so forth?”
Then host Kevin Newman pressed Humphry further and asked, “Are you saying in some cases people have a duty to die?” Flustered, Humphry replied,
“No, no. I think they have a responsibility and I don’t see — you see, assisted suicide is a crime everywhere except Oregon. Now, why if people want to die and justify it if the circumstances are right, why shouldn’t they go and save money at the same time?” [Transcript, Good Morning America, 11/3/98]
……..
Two Anchorage, Alaska, residents have filed a lawsuit in state Superior Court challenging an Alaska law prohibiting assisted suicide. Kevin Sampson, an AIDS patient, and “Jane Doe,” a physician with cancer, are the current plaintiffs in the case, however, their lawyer, Bob Wagstaff, has indicated that he hopes to have the case certified as a class action.
According to Wagstaff, the assisted suicide law violates the right to privacy provision of the Alaska Constitution. The suit aims to overturn the part of the manslaughter law which bans aiding another to commit suicide. “This case is not about doctors giving injections to patients. It‘s not about euthanasia,” Wagstaff told reporters. Rather, he said, it’s about patients ending their suffering by “self-administering” a lethal dose of medication. Wagstaff also revealed that he is accepting assistance from the Seattle-based, right-to-die group Compassion in Dying of Washington. [Anchorage Daily News, 12/16/98]